Anemia – Hemorrhage (Health Care / Medication Associated Condition): Introduction
:quality(80))
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Introduction
Overview and Implications
Anemia is a decrease in the number of red blood cells (RBCs),hematocrit(Hct), or hemoglobin (Hb) content. Anemia is not a diagnosis; it is a manifestation of an underlying disorder. Anemia can occur as the result of one or more of three basic mechanisms; blood loss, deficient erythropoiesis, and excessive hemolysis (Lichtin, 2017). The focus of this resource is on anemia related to acute blood loss (acute posthemorrhagic anemia) and hemorrhagic disorders due to circulating anticoagulants.
Acute post-hemorrhagic anemia secondary to Gastrointestinal (GI) Bleeding
Patients may have acute blood loss from GI bleeding. Nosocomial GI bleeding is source of preventable hospital morbidity and mortality (Herzig et al. 2013). Causes of upper GI bleeding include peptic ulcers, gastritis and inflammation of the GI lining from ingested materials. Ulcers are localized erosions of the mucosal lining of the digestive tract and they usually occur in the stomach or duodenum. Breakdown of the mucosal lining results in damage to blood vessels, which causes bleeding. Gastritis and inflammation of the GI lining may be caused by non-steroidal anti-inflammatory drugs (NSAIDs) and steroids (Lanza et al. 2009; Narum et al. 2014). In the ICU, stress-induced mucosal lesions are a risk factor for bleeding (McEvoy & Shander, 2013).
Acute GI bleeding will appear as vomiting of blood, bloody bowel movements or black, tarry stools. Vomited blood may look like coffee grounds. Other symptoms include fatigue, weakness, shortness of breath, abdominal pain, and pale appearance.
Risk Factors for nosocomial GI bleeding in ICU patients (Guillamondegui et al. 2008; Weinhouse, 2019):
- Universally accepted risk factors stress ulceration:
- Mechanical Ventilation for more than 48 hours
- Coagulopathy
- Other risk factors identified:
- shock
- sepsis
- spinal cord injury
- multiple trauma
- head trauma
- burns over 35 per cent of the total body surface area
- acute renal failure
- hepatic failure
- history of peptic ulcer disease
- history of upper GI bleed
- Organ transplantation
- Glucocorticoid therapy (when combined with other risk factors)
Hemorrhagic disorder due to circulating anticoagulants
Anticoagulation is the mainstay of medical treatment, prevention and reduction of recurrent venous thromboembolism, acute ischemic limbs, acute stroke, stroke prevention in patients with non-valvular atrial fibrillation, and it reduces the incidence of recurrent ischemic events and death in patients with acute coronary syndrome (Christos & Naples, 2016). Unfortunately, however the use of these medications carries significant risk of bleeding or hemorrhage.
Bleeding, or hemorrhagic disorder, is a possible side effect of anticoagulation therapy. (Carnovale et al. 2015). Anticoagulation therapy includes the use of warfarin (Coumadin), a Vitamin K antagonist, as well as the newer direct oral anticoagulants (DOACs) (Fernandez, 2015). Hemorrhage secondary to the use of vitamin K antagonists varies from one to 12 per cent per year, and is related to other risk factors. The risk of bleeding is highest in the initial few weeks of anticoagulation therapy (Cairns, 2011). As a drug category, anticoagulants are one of the top five drug types associated with patient safety incidents (Cousins, 2006).
Antithrombotic agents* are included on the Institute for Safe Medication Practice's (ISMP, 2018) high alert medication list due to the significant risk of causing life-threatening bleeding or thrombosis if the appropriate safe practices are not in place. This high risk is due to the complexity of administering this therapy:
- Selecting the appropriate agent and determining the appropriate dose
- Individual patient variability in response to therapy
- Timing of and use of the appropriate laboratory measures to monitor response
- Proper adjustment of dose based upon the laboratory parameters and/or clinical response
- The transition of patients from Heparin therapy to Warfarin
- Ensuring patient education and compliance
- Use of these agents in a variety of settings, by various practitioners, and within differing patient populations
- Interdisciplinary coordination needed between lab, pharmacy, nursing, medical staff, and dietary (Purdue University PharmaTAP, 2008)
*Antithrombotic agents, include:
- anticoagulants (e.g., warfarin, low molecular weight heparin, IV unfractionated heparin)
- Factor Xa inhibitors (e.g., fondaparinux, apixaban, rivaroxaban) direct thrombin inhibitors (e.g., argatroban, bivalirudin, dabigatran etexilate)
- thrombolytics (e.g., alteplase, reteplase, tenecteplase)
- glycoprotein IIb/IIIa inhibitors (e.g., eptifibatide)
Adverse drug events associated with anticoagulantscan be reduced by implementing recognized safe practices in high risk areas such as:Use Programmable Pumps and Independent Double-Checks for IV Anticoagulants,Prepare All Heparin Doses and Solutions in the Hospital Pharmacy, andProvide Coagulation Test Results Within Two Hours or at Bedside(IHI, 2020b).
Patients who are receiving anticoagulant therapy have increased risk of hemorrhage when undergoing medical and surgical procedures (Guidelines and Protocols Advisory Committee 2015). Bleeding that occurs in hospital is associated with increased morbidity, mortality, increased length of stay, increased health care costs and increased hospital readmission (Purdue University PharmaTAP, 2008; Herzig et al. 2013; McEvoy & Shander, 2013).
For additional information regarding anemia – hemorrhage associated with a medical or surgical procedure, please refer to theHospital Harm Improvement ResourceProcedure Associated Conditions: Anemia – Hemorrhage.
Goal
Reduce the incidence of hemorrhagic anemia or hemorrhagic disorders identified during a hospital stay, related to the health care delivered or therapeutic use of anticoagulants.
Table of Contents
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): Discharge Abstract Database
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): Importance to Patients and Families
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): Clinical and System Reviews, Incident Analyses
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): Measures
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): Success Stories
- Anemia – Hemorrhage (Health Care / Medication Associated Condition): References
Current page: https://www.healthcareexcellence.ca/en/resources/hospital-harm-is-everyones-concern/hospital-harm-improvement-resource
 (img: https://a-ca.storyblok.com/f/850807391887861/084049412e/general-image-three.jpg)
(img: https://a-ca.storyblok.com/f/850807391887861/084049412e/general-image-three.jpg)
Hospital Harm Improvement Resource
Patients expect hospital care to be safe and for most people it is. However, a small proportion of patients experience some type of unintended harm as a result of the care they receive.
The Canadian Institute for Health Information (CIHI) and Healthcare Excellence Canada (HEC) have collaborated on a body of work to address gaps in measuring harm and to support patient safety improvement efforts in Canadian hospitals.
The Hospital Harm Improvement Resource (improvement resource) was developed by HEC to complement the Hospital Harm measure developed by CIHI. It links measurement and improvement by providing evidence-informed practices that will support patient safety improvement efforts.
The purpose of measuring quality and safety is to improve patient care and optimize patient outcomes. The Hospital Harm measure should be used in conjunction with other sources of information about patient safety, including patient safety reporting and learning systems, chart reviews or audits, Accreditation Canada survey results, patient concerns and clinical quality improvement process measures. Together, this information can inform and optimize improvement initiatives.
The improvement resource is a compilation of guidance linked to each of the clinical groups within the Hospital Harm measure to help drive changes that will make care safer. Through research and consultation with clinicians, experts, and leaders in quality improvement (QI) and patient safety, the improvement resource is intended to make information on improving patient safety easily available, so teams spend less time researching and more time optimizing patient care.
Using the improvement resource
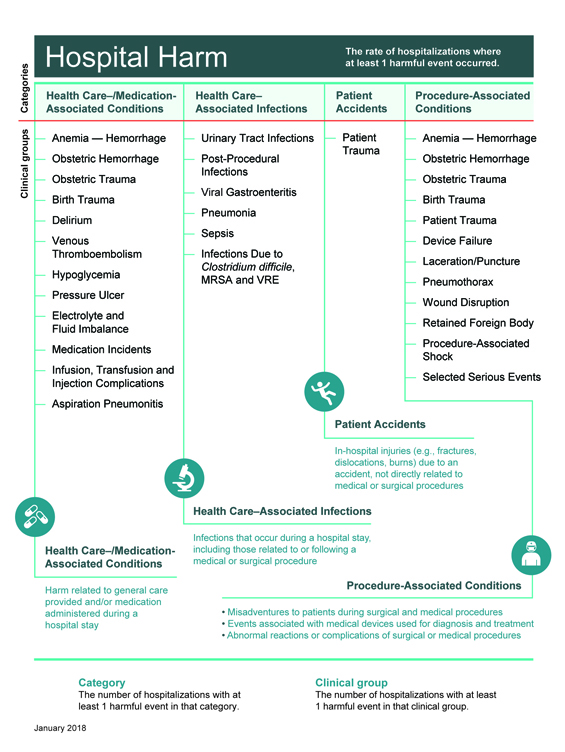
The layout of the improvement resource reflects the framework of the Hospital Harm measure (Figure 1) and focuses on actions that can be taken to decrease the likelihood of harm. The measure includes four major categories of harm; within each category is a series of individual clinical groups, or types of harm, each of which connects to evidence-informed practices for improvement.
For each clinical group, the improvement resource provides the following:
- an overview of the clinical group and goal for improvement
- implications for patients experiencing the type of harm and their importance to patients and family
- guidance for clinical and system reviews and incident analyses, including a list of resources specific to the clinical group
- guidance on measuring improvement
- success stories from organizations
- references.
Figure 1: Hospital Harm Measure Framework
 (img: https://a-ca.storyblok.com/f/850807391887861/1625902acd/hh-framework.jpg)
(img: https://a-ca.storyblok.com/f/850807391887861/1625902acd/hh-framework.jpg)
Definitions
As patient safety evolves it is important to be clear on the meaning and differences of specific words. For the purposes of the Hospital Harm measure, the following definitions apply:
- Harm:An unintended outcome of care that may be prevented with evidence-informed practices and is identified and treated in the same hospital stay.
- Occurrence of harm:Harmful event is synonymous with occurrence of harm.
- Hospital Harm Measure:Acute care hospitalizations with at least one unintended occurrence of harm that could be potentially prevented by implementing known evidence-informed practices.
For harm to be included in the measure, it must meet the following three criteria.
- It is identified as having occurred after admission and within the same hospital stay.
- It requires treatment or prolongs the patient's hospital stay.
- It is one of the conditions from the 31 clinical groups in the Hospital Harm Framework.
If you have any feedback or suggestions for the Improvement Resource, please send your ideas toinfo@hec-esc.ca
Table of Contents
- How to Use the Hospital Harm Measure for Improvement
- General Patient Safety Quality Improvement and Measurement Resources
- Learning from Harm
Resources
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Discharge Abstract Database
Discharge Abstract Database (DAD) Codes included in this clinical category:
A01: Anemia – Hemorrhage (Health Care/Medication Associated Condition)
Concept | Hemorrhagic anemia or hemorrhagic disorders that require(s) blood transfusion, identified during a hospital stay, related to the health care delivered or therapeutic use of anticoagulants |
Notes |
|
Selection criteria | |
D62 | Identified as diagnosis type (2) AND Y44.2 in the same diagnosis cluster |
Exclusions | Y60–Y84 in the same diagnosis cluster |
Codes | Code descriptions |
D62 | Acute posthemorrhagic anemia |
D68.3 | Hemorrhagic disorder due to circulating anticoagulants |
Additional Codes | Inclusions |
Y44.2 | Drugs, medicaments and biological substances causing adverse effects in therapeutic use, anticoagulants |
Additional Codes | Exclusions |
Y60-Y84 | Complications of medical surgical care (refer toAppendix Aof theHospital Harm Indicator General Methodology Notes) |
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Importance to Patients and Families
Hemorrhage is understandably alarming to patients and families. Not only may it be life-threatening, it complicates care and prolongs hospitalization. Anticoagulants such as warfarin and heparin are powerful medications that save lives and prevent further harm. This group of medications also has the potential to cause serious harm if not taken carefully. Patients who are knowledgeable about their medication therapy can help to reduce the risk of adverse drug events (IHI, 2020a).
Patient Stories
Dennis Quaid Recounts Twins' Drug Ordeal
[The twins] were supposed to have been given a pediatric blood thinner called Hep-lock to flush out their IV lines and prevent blood clots. But instead, they had been given two doses of Heparin, the adult version of the drug, which is 1,000 times stronger…. "It was ten units that our kids are supposed to get. They got 10,000. And what it did is, it basically turned their blood to the consistency of water, where they had a complete inability to clot. And they were basically bleeding out at that point."
"There was blood oozing out of little blood draws on their feet, and things like that, you know, through band-aids," he adds….
And to make matters worse the same avoidable mistake had occurred a year earlier at Methodist Hospital in Indianapolis. Six infants were given multiple adult doses of Heparin instead of the pediatric version; three of the infants survived, three did not….
Popular Blood Thinner Causing Deaths, Injuries at Nursing Homes
Some facilities fail to properly oversee Coumadin. Too much can cause bleeding; too little, clots. Nursing homes are "a perfect setup for bad things happening," one expert says….
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Clinical and System Reviews, Incident Analyses
Given the broad range of potential causes of anemia - hemorrhage,clinical and system reviews should be conducted to identify potential causes and determine appropriate recommendations.
Occurrences of harm are often complex with many contributing factors. Organizations need to:
- Measure and monitor the types and frequency of these occurrences.
- Use appropriate analytical methods to understand the contributing factors.
- Identify and implement solutions or interventions that are designed to prevent recurrence and reduce risk of harm.
- Have mechanisms in place to mitigate consequences of harm when it occurs.
To develop a more in-depth understanding of the care delivered to patients, chart audits, incident analyses and prospective analyses can be helpful in identifying quality improvement opportunities. Links to key resources forconducting chart auditsandanalysis methodsare included in theHospital Harm Improvement Resources Introduction.
If your review reveals that your cases of anemia - hemorrhage are linked to specific processes or procedures, you may find these resources helpful:
- Institute for Safe Medication Practices (ISMP).www.ismp.org
- British Columbia.BCGuidelines.ca
- National Blood Authority Australia.Patient Blood Management.
- NATA, Network for the Advancement of Patient Blood Management, Haemostasis and Thrombosis.
- Thrombosis Canada.Clinical Guides.
- American Society of Health-System Pharmacists (ASHP): Gastrointestinal Stress Ulcer Prophylaxis (pending)https://www.ashp.org/pharmacy-practice/policy-positions-and-guidelines/browse-by-document-type/therapeutic-guidelines
- Stress Ulcers in the Intensive Care Unit: Diagnosis management and Prevention(Weinhouse, 2020)www.uptodate.com
- Institute for Healthcare Improvement (IHI):
- How-to guide: prevent harm from high-alert medications. 2012.http://www.ihi.org/resources/Pages/Tools/HowtoGuidePreventHarmfromHighAlertMedications.aspx
- Changes: Reduce adverse drug events involving anticoagulants. 2020.http://www.ihi.org/resources/Pages/Changes/ReduceAdverseDrugEventsInvolvingAnticoagulants.aspx
- Anticoagulant tool kit: Reducing adverse drug events & potential adverse drug events with unfractionated heparin, low molecular weight heparins and warfarin. 2008http://www.ihi.org/resources/pages/tools/anticoagulanttoolkitreducingades.aspx
- Joint Commission -National Patient Safety Goalto reduce the likelihood of patient harm associated with the use of anticoagulation therapy (Joint Commission, 2018).
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Measures
Vital to quality improvement is measurement, and this applies specifically to implementation of interventions. The chosen measures will help to determine whether an impact is being made (primary outcome), whether the intervention is actually being carried out (process measures), and whether any unintended consequences ensue (balancing measures).
In selecting your measures, consider the following:
- Whenever possible, use measures you are already collecting for other programs.
- Evaluate your choice of measures in terms of the usefulness of the final results and the resources required to obtain them; try to maximize the former while minimizing the latter.
- Try to include both process and outcome measures in your measurement scheme.
- You may use different measures or modify the measures described below to make them more appropriate and/or useful to your particular setting. However, be aware that modifying measures may limit the comparability of your results to others.
- Posting your measure results within your hospital is a great way to keep your teams motivated and aware of progress. Try to include measures that your team will find meaningful and exciting (IHI, 2012).
Anemia – Hemorrhage (Health Care / Medication Associated Condition): Success Stories
We are looking for an improvement success story related to Anemia - Hemorrhage. If you have one you would like to share, please contact the Canadian Patient Safety Institute atinfo@hec-esc.ca.
Anemia – Hemorrhage (Health Care / Medication Associated Condition): References
Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter.Cn J Cardiol. 2011; 27 (1), 74-90. doi: 10.1016/j.cjca.2010.11.007.https://www.onlinecjc.ca/article/S0828-282X%2810%2900008-5/fulltext
Carnovale C, Brusadelli T, Casini ML. Drug-induced anaemia: a decade review of reporting to the Italian Pharmacovigilance data-base.Int Clin J Pharm. 2015, 37 (1), 23-26. doi: 10.1007/s11096-014-0054-3
Christos S, Naples R. Anticoagulation reversal and treatment strategies in major bleeding: Update 2016.West J Emerg Med. 2016; 17 (3): 264-70. doi: 10.5811/westjem.2016.3.29294.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899056/
Cousins D, Harris, Safe Medication Practice Team.Risk assessment of anticoagulation therapy. National Patient Safety Agency; 2006.https://www.sps.nhs.uk/wp-content/uploads/2018/02/NRLS-0233-Anticoagulant-tssessment-2006-01-v1.pdf
Fernández CS, Formiga F, Camafort M, et al. Antithrombotic treatment in elderly patients with atrial fibrillation: a practical approach.BMC Cardiovasc Disord. 2015; 15: 143. doi: 10.1186/s12872-015-0137-7.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4632329/
Erratum: Fernández CS, Formiga F, Camafort M, et al. Erratum: Antithrombotic treatment in elderly patients with atrial fibrillation: a practical approach.BMC Cardiovasc Disord. 2015; 15: 157. doi: 10.1186/s12872-015-0150-x.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4653852/
Guillamondegui OD, Gunter OL Jr, EAST Practice Management Guidelines Committee.Practice management guidelines for stress ulcer prophylaxis. Chicago, IL: Eastern Association for the Surgery of Trauma; 2008.https://www.east.org/education/practice-management-guidelines/stress-ulcer-prophylaxis
Herzig SJ, Rothberg MB, Feinbloom DB, et al. Risk factors for nosocomial gastrointestinal bleeding and use of acid-suppressive medication in non-critically ill patients.J Gen Intern Med.2013; 28 (5): 683-690. doi: 10.1007/s11606-012-2296-x.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3631055/
Institute for Healthcare Improvement (IHI). How-to Guide: Prevent Harm from High-Alert Medications. Cambridge, MA: IHI; 2012. http://www.ihi.org/resources/Pages/Tools/HowtoGuidePreventHarmfromHighAlertMedications.aspx
Institute for Healthcare Improvement (IHI).Educate Patients to Manage Warfarin Therapy at Home.Cambridge, MA: IHI; 2020a. http://www.ihi.org/resources/Pages/Changes/EducatePatientstoManageWarfarinTherapyatHome.aspx
Institute for Healthcare Improvement (IHI).Changes: Reduce adverse drug events involving anticoagulants.Cambridge, MA: IHI; 2020b.http://www.ihi.org/resources/Pages/Changes/ReduceAdverseDrugEventsInvolvingAnticoagulants.aspx
Institute for Safe Medication Practices (ISMP). ISMP list of high-alert medications in acute care settings. Horsham, PA; ISMP: 2018.https://www.ismp.org/sites/default/files/attachments/2018-08/highAlert2018-Acute-Final.pdf
Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications.Am J Gastroenterol. 2009; 104 (3), 728-738. doi: 10.1038/ajg.2009.115.
Lichtin AE. Etiology of anemia.Merck Manual. 2017.www.msdmanuals.com/professional/hematology-and-oncology/approach-to-the-patient-with-anemia/etiology-of-anemia
McEvoy MT, Shander A. Anemia, bleeding, and blood transfusion in the intensive care unit: causes, risks, costs, and new strategies.Am J Crit Care. 2013; 22 (6 Suppl): eS1-13. doi: 10.4037/ajcc2013729.http://ajcc.aacnjournals.org/content/22/6/eS1.long
Narum S, Westergren T, Klemp M. Corticosteroids and risk of gastrointestinal bleeding: a systematic review and meta-analysis.BMJ Open. 2014, 4 (5): e004587. doi: 10.1136/bmjopen-2013-004587.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4025450/
Purdue University PharmaTAP.Anticoagulant tool kit: Reducing adverse drug events & potential adverse drug events with unfractionated heparin, low molecular weight heparins and warfarin. Indianapolis, IN: Purdue University PharmaTAP: 2008.http://www.ihi.org/resources/pages/tools/anticoagulanttoolkitreducingades.aspx
Weinhouse GL. Stress ulcer prophylaxis in the intensive care unit.UpToDate.2018.https://www.uptodate.com/contents/stress-ulcer-prophylaxis-in-the-intensive-care-unit